Earlier this year, we studied guidance from the World Health Organisation (WHO), UK Government, Public Health England (PHE), The International Pharmaceutical Federation (FIP) and spoken with colleagues in Europe, to provide a pragmatic approach to the use of PPE and other measures (learn more). Below is an update.
Public control measures in community pharmacy
Ensure all members of the public and staff adhere to the 2m social distancing guidance wherever possible:
- Display posters advising members of the public that they should not be entering community pharmacies if they have any COVID-19 symptoms.
- Individuals should maintain 2m distance when queuing
- Individuals must wear a face-covering unless requested to remove it temporarily as part of a pharmacist consultation (or unable to wear a mask for medical or other reasons set out in government guidance).
- Pharmacies should restrict the number of customers and patients allowed into the pharmacy to support social distancing. Members of the public may need to queue outside to allow this.
- Once a maximum number of patients and customers has been reached, operate a one-in-one-out process
- Floor markings at 2m intervals inside the store and in the queuing area outside can be of benefit.
Physical Barriers
- Retractable tape barriers or other measures can be used inside the pharmacy to direct queues appropriately and help enforce social distancing.
- Clear Perspex or glass screens provide a physical barrier at the counter to reduce exposure to the virus and are recommended by the WHO.
- Consultation rooms/treatment areas may need to be modified to allow suitable social distancing and management of vaccination services (see PSNC).
Fluid-resistant surgical masks (FRSMs)
PHE guidance published on 16th September 2020 stated that staff working in primary and community healthcare facilities should wear Type I or Type II facemasks in areas which could not be made COVID-19 secure through social distancing. The PDA is pleased to note that the DHSC has now added community pharmacies to those NHS providers which can order all PPE requirements via the PPE portal.
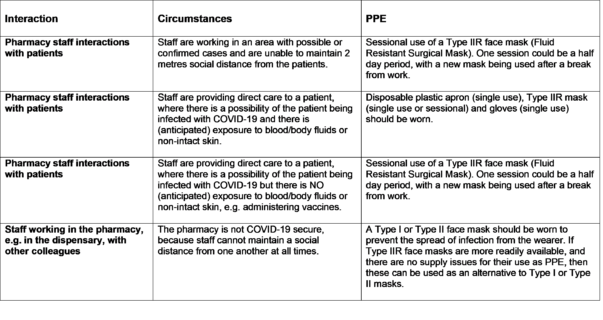 Taken from the PSNC website on 02.10.20
Taken from the PSNC website on 02.10.20
The Employers responsibility in law
This is an area where healthcare guidance is not the only governing factor – employers have a regulatory duty under the Health & Safety at Work Act to ensure that their workers can do their job safely and that appropriate PPE is provided. Should an employee come to harm as a result of working unprotected, their employer would have a legal obligation to report this under RIDDOR regulations and we urge all pharmacist employees to bring such cases to their employers notice as and when this occurs.
The PDA advice
As key members of the teams keeping the last remaining walk-in access to frontline NHS services running, community pharmacy staff need to be adequately protected. It is important that measures are taken to ensure that risks to this crucial sector of the workforce are mitigated as far as possible, be that by the NHS or pharmacy employers. The NHS has opened the PPE ordering portal to pharmacies which should address the significant sourcing issues which pharmacies experienced previously. However, the primary responsibility for the protection of employee’s in the workplace lies with the employers and those employers who do not take their responsibilities under Health and Safety Legislation seriously during the crisis, run the risk of action being taken against them under the H&S legislation once the crisis is over.
Risk managing your safety
Over and above the use of Perspex screens and the wearing of face masks, the PDA shares advice on Covid-19 infection mitigation, much of this advice is based on successful initiatives used in pharmacies in other countries and remains worthy of consideration as we head into the winter season.
Disposable gloves
Whilst PHE does not feel that any further PPE is required in community pharmacy, the PDA view is that the risk of transmission of virus fragments via surfaces including seating, counters, bank card machines, money and pens provided for signing prescriptions as well as the stock that is handed over by a member of the public during a transaction makes the wearing of disposable gloves prudent. Regular handwashing is important for public protection but expecting staff to go and wash their hands after each potentially risky contact is impractical. Modest quantities of gloves and aprons will be available to community pharmacies via the PPE portal.
Clothes worn in the pharmacy
Clothes worn during the working day in a pharmacy could very easily attract and retain virus particles. Thought should be given to wearing a set of clothes in the workplace, which is then immediately removed and laundered once returning home. Different attire should then be worn at home, so as to protect other members of the family where appropriate.
Staffing; longer hours and introduction of shift patterns
In some European countries, the closure of general practice to routine face to face consultations and the resultant increase in attendance at community pharmacies has resulted in additional government support to allow pharmacies to remain open for extended hours. Funding has facilitated longer hours of opening and increases in the numbers of pharmacy team members. Business continuity and resilience has been enhanced by the pharmacy workforce splitting into two teams working early or late shift, with no crossover. This has reduced the risk of coronavirus infection spreading throughout the entire workforce in a particular pharmacy.
Cleaning regimes
Routine cleaning of high-risk areas such as door handles, counters, pens, shopping baskets, all counters as well as communal staff areas should be adopted. Many retail outlets are enabling members of the public to wipe down and clean their own shopping basket handles.
Handling of used PPE
All types of PPE must be donned and removed, taking care not to introduce contamination in the process. In particular, when removing masks or gloves care should be taken so as not to touch the outside surface which may carry virus particles and ensure items are disposed of safely.
Infection control damaged by employer practices
The PDA trusts that the clear recent guidance and the ability of employers to order all PPE requirements via the PPE portal will do away with the shameful practices which occurred earlier in the pandemic. Concerns now switch to the disgraceful practice of booking unmanageable numbers of daily vaccination appointments in single pharmacist locations where the RP is expected to manage all of the dispensary checking, countertrade and walk-in advice as well.
The PDA is always keen to receive information about unacceptable employer practices and will raise issues with regulatory and other bodies as appropriate. We encourage members to let us know about any concerns.
Related links
- Personal Protective Equipment – rationale and recommendations for a pragmatic approach
- World Health Organisation -Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19), March 2020
- Cabinet Office & DHSC
- Public Health England
- PSNC – Personal protective equipment, staff safety and security
- HSE RIDDOR reporting of COVID-19
- PPE portal: how to order COVID-19 personal protective equipment (PPE)
- FIP guidelines