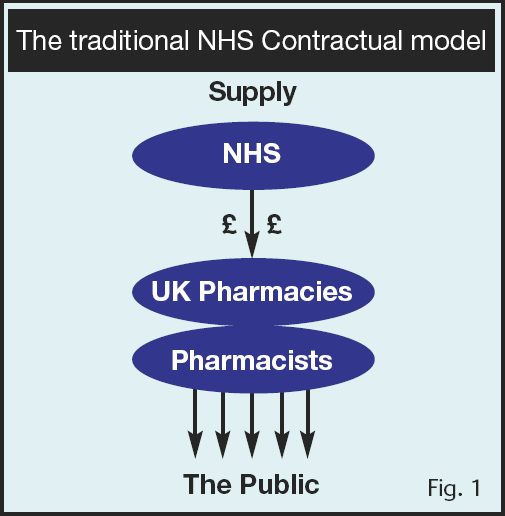
As a direct consequence of this, our pharmacist fore fathers established employer led organisations like the National Pharmacy Association, the Pharmaceutical Services Negotiating Committee and the Company Chemists Association to ensure that their interests could be well looked after. Following the launch of the National Health Service, the pharmacy representative bodies ensured that contracts with the NHS were established, so as to provide pharmacy owners with a fair return on their investment. This was entirely proper as the operation of a pharmacy requires owners to invest and risk their own funds in the physical facility and for the expensive medicines which the NHS requires to be supplied to the public. This is what one might call the traditional ‘bricks and mortar’ NHS contractor model – so far so good.
A century later, there are major differences in the pharmacy landscape. Today, more than 90% of pharmacists are either employees or self-employed locums working in the community, hospital or primary care setting. Pharmacy ownership is now dominated by large multiples and independent pharmacy ownership is decreasing. These days, the cost of pharmacy ownership has put it beyond the reach of many pharmacists.
In addition to this, the role of the pharmacist is significantly different. There is no longer a need for pharmacists to be manually involved in the ‘compounding’ of medicines. The very fabric of the pharmacy service, which traditionally has been rooted in the manufacture and supply of medicines, is now moving towards the provision of services to the public and this is where the future lies.
And herein lies the problem, whilst it is easy to understand why the appropriate body to enjoy an NHS contract for the supply of medicines to the public is the owner of pharmacy, it becomes less so if one considers the provision of services. For, whilst the supply of medicines requires and deserves a satisfactory return on its financial risk and investment, the provision of services is largely a professional and intellectual investment that has to be made by the person undertaking the task i.e. by the individual pharmacist.
This then begs the question that if it is the ‘bricks and mortar’ contractor that receives the payment from the NHS, then what return does the individual pharmacist receive on this intellectual investment and upon the associated risk of providing the service?
It is our view that whilst the traditional NHS contractor model (seen in fig. 1), may well work for the medicines supply, it does not work for the provision of services. This is much more than an issue of fairness, we believe that the old ‘bricks and mortar’ remuneration model causes a ‘disconnect’ when the new services are being provided which results in problems for patients, for pharmacists and also for the relationship between employers and pharmacists. (See fig. 2).
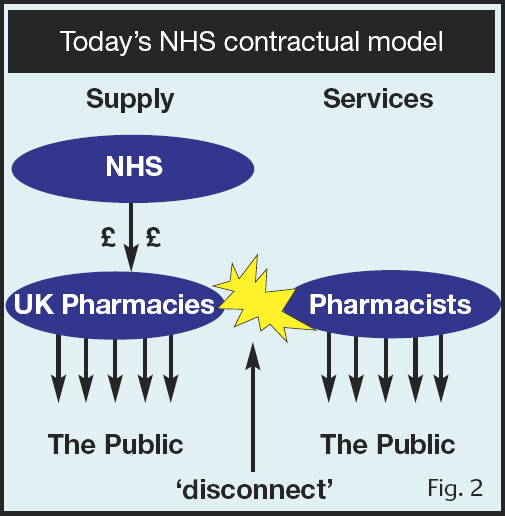
We are concerned that some employers see these services as no more than a cash generator. Meanwhile, pharmacists at the coal face who are actually delivering the service will want to take a much greater interest in the quality and professional integrity of the service and these considerations clash with the commercial prerogative. Sadly, because of the master servant relationship that now dominates pharmacy, many employee and locum pharmacists are relentlessly driven to deliver MURs despite not being provided with an appropriate working environment (in terms of availability of support staff) nor, in many situations, even having patients that genuinely need to have an MUR undertaken.
We believe that unless this ‘disconnect’ is addressed, then it will harm the agenda for rolling out future pharmacist led services. We must accept that an important requirement of patients and Society generally, is that pharmacists, who regardless of employer or environment can be professionally independent in terms of their practice.
These are more than just theoretical concerns, the table below shows the symptoms of this disconnect as they relate to the provision of MURs.
- MURs not taken up widely
- Complaints from GPs about poor quality MURs being received
- Complaints from patients
- Creative methods being used to drive volumes
- MURs being driven not by need but by targets
So what do the employers say?
Here are the contents of some company communications to pharmacists;
- “Some pharmacists don’t agree that MURs are part of their role – well guess what, at £27 a pop, MURs represent £10,800 bottom line – they are!”
- “If your pharmacists still refuse or are not hitting their MUR targets then they need to be managed accordingly. I need to understand, by close of play today, what you, as leaders of your businesses are going to do by 10.00am Thursday.”
- “In my previous job before I became area manager I was targeted to sell tyres and I see no difference with targeting MURs.”
So what do the pharmacists say?
Here is a small sample of views that we have had from pharmacists;
- “I have been harassed by area managers who phone me at home when ill due to pregnancy demanding my return to the pharmacy to do more MURs.”
- “Community pharmacy is all I have ever wanted to do. However, ridiculous MUR targets have changed all that. I frequently feel inadequate and stressed about it. I never thought that after five years of training I could expect an emotional slap on the wrist for not achieving 12 MURs every week..”
- “The stress placed on us from area managers in North Wales with regards to MURs is ridiculous. Constant harrasment via e-mail, daily phone calls etc is the norm and we are made to feel like poor pharmacists if we do not conduct at least 12 a week regardless of patient type.”
At the PDA, we believe in a fundamental principle, that the closer the pharmacists responsibility is to the patient, the safer it is for the patient and the better it is for the pharmacist. We also argue that the intellectual investment and risk taken by the pharmacist in the provision of services should be rewarded by an appropriate return.
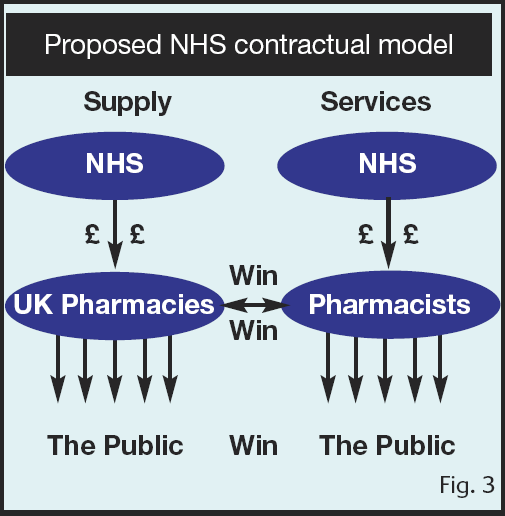
We want to see the creation of an individual pharmacist held NHS contract which would be used to fund the provision of professionally led services to patients. We argue that if the correct WIN-WIN arrangements can be made, then this new form of contract, held by individual pharmacists need not threaten the income of the traditional ‘bricks and mortar’ contractor, indeed, if organised properly, then it could even increase it. If, for example new services where provided by individual pharmacists, but from the community pharmacy setting, then pharmacists could make arrangements to ‘hire’ the facilities already provided by the ‘bricks and mortar’ contractors such as consultation rooms, appointment booking services and various other establishment based facilities. (See fig. 3).
These views have been discussed by the PDA for at least three years, however, every good idea needs the right timing. It is encouraging to see that the idea of the individual pharmacist contractor is now gaining momentum. At the recent PDA conference in Spring 2010, the Chief Pharmacist for Scotland, Professor Bill Scott addressed the PDA delegates and described the direction of travel in Scotland. He indicated to PDA members that he was very supportive of the PDA’s proposals.
According to Bill Scott, the current pharmacy owner centred funding model, with its focus on prescription volume and drug purchasing profits was a “rate limiting step to pharmacists further clinical development”. It placed corporate values against those of individual practitioners and lacked continuity of pharmaceutical care. It created conflicts of interest and acted as a barrier to full involvement with other healthcare professionals. “GPs insult you by calling you shopkeepers and you wonder why it is an uphill struggle to develop the profession. This problem exists because of the current contracting model.” He said.
“There is a tendency to think of prescriptions as pound notes rather than in terms of patient outcomes.”
“I would like to see the contract separated into two parts, both to be delivered from a registered pharmacy.
The first would have the NHS contracting with pharmacy owners for premises, stock, equipment and support staff. The second would involve NHS contracts with individual pharmacists to provide clinical pharmaceutical services.”
Bill explained that the new model would boost pharmacists’ professionalism and independence, would remove perverse incentives and by focusing on pharmaceutical care, would encourage partnership working and ultimately support continuity of patient care. This would provide a strong basis upon which to build a future for clinical developments.
To the delight of PDA conference delegates Bill said “The ostriches must take their heads out of the sand. The current contracting model is not fit for the 21st Century so let’s widen the debate and develop the clinical and business model. By using our professionalism to put patients first, we may come out with something better than what we have now.”
In concluding the presentation, Bill invited the PDA to continue to actively contribute to the debate and to not only seek, but to demand a new individual pharmacist based NHS contracting model for all pharmacists in the UK.
Where to from here?
In its mission to establish this new kind of NHS contract, PDA members are urged to use every opportunity to influence those that they can so as to assist with the development of this programme. For the PDA to be successful in its central discussions with the government and others, then pharmacists at the coalface must believe in and demand the opportunity to develop this new concept and create the groundswell of opinion. With the new financial situation facing the nation, we believe that the time is right to engineer a situation where through a fundamental adjustment to the flow of NHS funds, the profession can deliver more for patients with improved value for money. Indeed, such discussions have already commenced.
Please watch out for details of our activities and any specific calls for membership support.